Related Posts
Why Old Tractors Still Earn Respect on the Farm An old tractor doesn’t shout for attention. It doesn’t blink lights…

Brigade Secunderabad is emerging as one of the most anticipated premium residential developments in Hyderabad. Designed to meet the expectations of…

In recent years, a significant shift has occurred in the digital landscape as users increasingly delete multiple standalone apps in…

Keeping your vehicle in top condition requires the expertise of a trusted and experienced mechanic in Chatham. Whether you use…
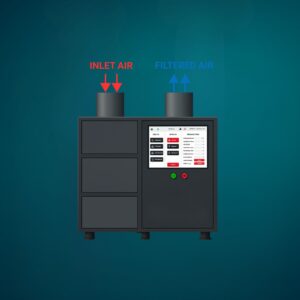
Ever wonder why big factories and workshops keep coming back to the same name for cleaner air? It’s not luck—it’s…

Core gameplay in most MMOs typically provides some source of passive income; FFXIV is no exception – quests offer Gil…
The First Time You Trust a Tractor With Your Land A tractor is not something you admire from a distance.…
Windows play a much bigger role in a home or commercial space than most people realize. They control natural light,…
Rings often hold more than just material value. They represent love, milestones, memories, and sometimes generations of family history. Whether…
A clean office is not just about appearances; it directly impacts productivity, employee well-being, and the way a business is…