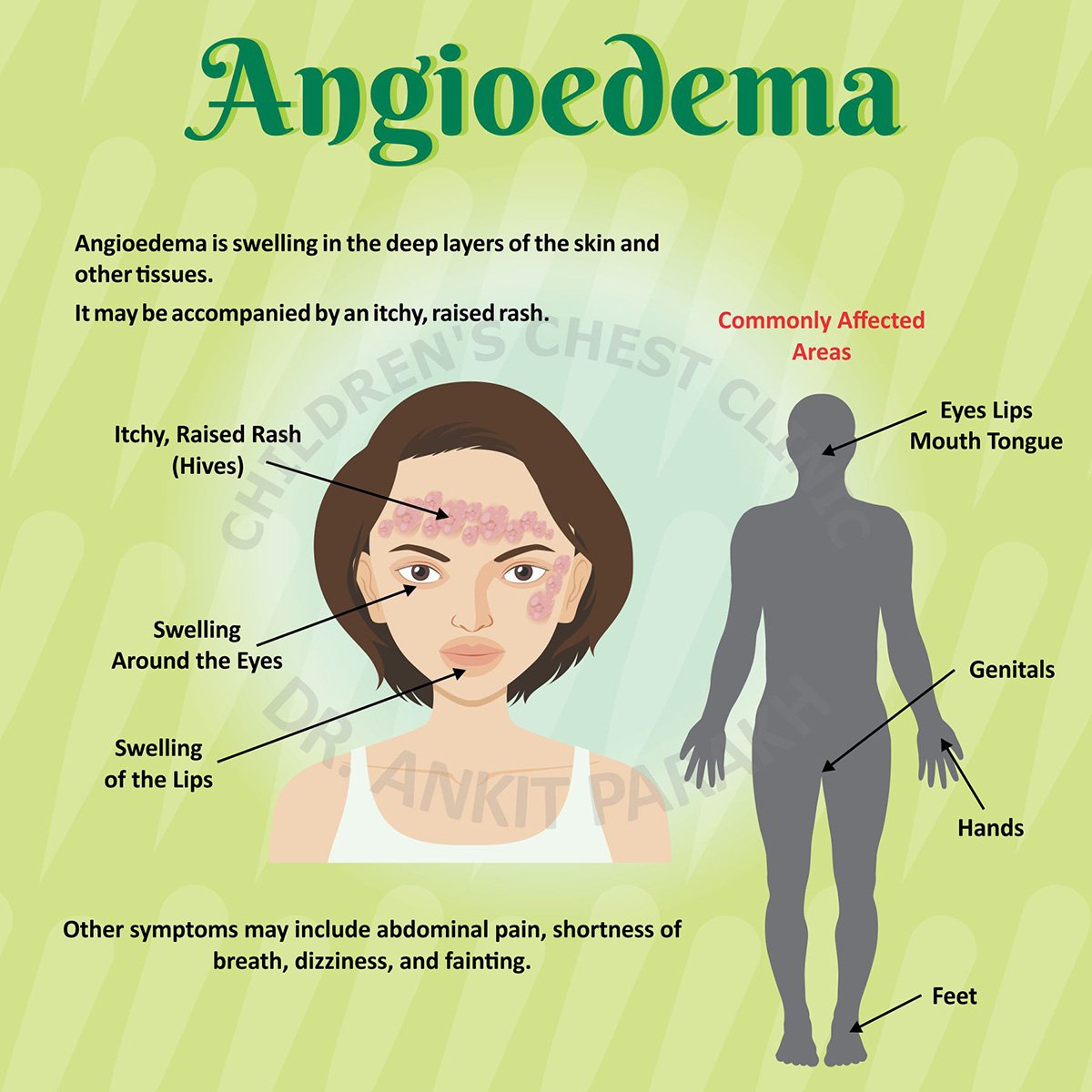
Angioedema is a condition characterized by sudden, localized swelling beneath the skin, often affecting areas like the face, lips, throat, or extremities. It can be triggered by allergic reactions, medications, hereditary factors, or other underlying causes. The swelling can be uncomfortable or, in severe cases, life-threatening if it obstructs airways. Effective treatment depends on identifying the cause and tailoring interventions to the patient’s needs.
Understanding Angioedema and Its Causes
Angioedema results from the release of histamine or bradykinin, leading to increased vascular permeability and fluid leakage into tissues. Common types include:
- Allergic Angioedema: Triggered by allergens like foods, insect stings, or medications.
- Hereditary Angioedema (HAE): Caused by genetic mutations affecting C1-inhibitor protein, leading to uncontrolled bradykinin production.
- Drug-Induced Angioedema: Often linked to ACE inhibitors or NSAIDs.
- Idiopathic Angioedema: When the cause is unknown.
Symptoms include swelling, redness, and sometimes pain or itching. In severe cases, swelling in the throat can cause breathing difficulties, requiring urgent care.
General Treatment Approaches
The treatment of angioedema varies based on its type, severity, and underlying cause. Below are the primary strategies:
1. Avoiding Triggers
Identifying and avoiding triggers is critical, especially for allergic or drug-induced angioedema. For example, patients allergic to certain foods or medications should avoid them. For drug-induced cases, discontinuing the offending medication (e.g., ACE inhibitors) often resolves symptoms. Patients should consult their healthcare provider before stopping any prescribed medication.
2. Antihistamines
For allergic angioedema, antihistamines are the first-line treatment. They block histamine, reducing swelling and itching. Non-sedating antihistamines like cetirizine or loratadine are commonly prescribed. In severe cases, higher doses or sedating antihistamines like diphenhydramine may be used. Antihistamines are less effective for hereditary or bradykinin-mediated angioedema.
3. Corticosteroids
Corticosteroids, such as prednisone, are used to reduce inflammation in allergic or idiopathic angioedema. They are often prescribed for short-term use in acute attacks, particularly when antihistamines alone are insufficient. Long-term use is avoided due to side effects like weight gain or osteoporosis.
4. Epinephrine
In life-threatening cases, such as angioedema causing airway obstruction, epinephrine is administered immediately. It rapidly reduces swelling and stabilizes breathing. Patients with a history of severe allergic reactions may carry an epinephrine auto-injector (e.g., EpiPen) for emergencies.
5. Targeted Therapies for Hereditary Angioedema
HAE requires specialized treatments because it is not histamine-mediated. Options include:
- C1-Inhibitor Concentrates: Drugs like Berinert or Cinryze replace deficient C1-inhibitor, controlling bradykinin production.
- Bradykinin Receptor Antagonists: Icatibant (Firazyr) blocks bradykinin activity, reducing swelling.
- Kallikrein Inhibitors: Lanadelumab (Takhzyro) prevents excessive bradykinin production and is used for long-term prevention.
- Androgens: Danazol may be used in some cases to increase C1-inhibitor levels, though it is less common due to side effects.
These therapies are effective for acute attacks or as prophylactic treatment in patients with frequent episodes.
Role of Cephalexin Capsules in Angioedema Management
Cephalexin capsules, a first-generation cephalosporin antibiotic, are not a direct treatment for angioedema but may play a role in specific scenarios. Cephalexin is primarily used to treat bacterial infections, such as skin or soft tissue infections. In the context of angioedema, it may be relevant in the following situations:
- Infection-Associated Angioedema: Rarely, bacterial infections (e.g., cellulitis) can trigger or exacerbate angioedema by causing localized inflammation. If a bacterial infection is confirmed, cephalexin capsules may be prescribed to treat the underlying infection, indirectly alleviating angioedema symptoms. For example, a patient with facial angioedema caused by an infected wound may benefit from cephalexin to resolve the infection and reduce swelling.
- Preventing Complications: In cases where angioedema leads to skin breakdown or secondary infections, cephalexin capsules can prevent or treat these complications. The typical dosage is 250–500 mg every 6–12 hours, depending on the infection’s severity, as prescribed by a healthcare provider.
- Caution with Cephalexin: Cephalexin itself can, in rare cases, cause allergic reactions, including angioedema, particularly in patients with a history of penicillin or cephalosporin allergies. Patients should report any new swelling or rash while taking cephalexin capsules to their doctor immediately.
While cephalexin capsules are not a standard treatment for angioedema, their use in managing infection-related triggers underscores the importance of addressing underlying conditions to control symptoms effectively.
Emergency Management
Severe angioedema, especially involving the throat or tongue, is a medical emergency. Immediate steps include:
- Administering epinephrine if an allergic cause is suspected.
- Securing the airway through intubation or tracheostomy if swelling obstructs breathing.
- Administering oxygen and IV fluids to stabilize the patient.
Patients with HAE may require C1-inhibitor concentrates or icatibant in emergencies, as antihistamines and corticosteroids are ineffective for bradykinin-mediated swelling.
Long-Term Management and Prevention
For patients with recurrent angioedema, long-term strategies focus on prevention and reducing attack frequency:
- Prophylactic Medications: For HAE, drugs like lanadelumab or C1-inhibitor concentrates are used to prevent attacks. For chronic idiopathic angioedema, daily antihistamines or low-dose corticosteroids may be considered.
- Lifestyle Modifications: Avoiding known triggers, managing stress, and maintaining a healthy diet can reduce the likelihood of attacks.
- Patient Education: Patients should be educated about their condition, including how to recognize early symptoms and when to seek emergency care. Those with HAE may benefit from a medical alert bracelet.
Complementary and Supportive Therapies
While not primary treatments, complementary therapies can support angioedema management:
- Cool Compresses: Applying cool compresses to swollen areas can reduce discomfort and inflammation.
- Hydration and Nutrition: Staying hydrated and avoiding dietary triggers (e.g., shellfish in allergic angioedema) can help.
- Stress Management: Stress can exacerbate angioedema, so techniques like yoga or meditation may be beneficial.
When to Seek Medical Attention
Patients should seek immediate medical care if they experience:
- Swelling in the throat, tongue, or airways.
- Difficulty breathing or swallowing.
- Persistent or worsening symptoms despite treatment.
For non-emergent cases, consulting an allergist or immunologist can help identify triggers and develop a personalized treatment plan.
Conclusion
The best treatments for angioedema depend on its cause and severity. Allergic angioedema responds well to antihistamines, corticosteroids, and epinephrine in emergencies, while hereditary angioedema requires targeted therapies like C1-inhibitor concentrates or bradykinin antagonists. Cephalexin capsules may be used in rare cases where bacterial infections contribute to angioedema, but they are not a primary treatment. Avoiding triggers, using prophylactic medications, and seeking timely medical care are key to managing this condition effectively. By understanding the underlying mechanisms and tailoring treatments to the patient’s needs, healthcare providers can help patients achieve better outcomes and improve their quality of life.
